Abstract

Introduction- Untreated Graft Failure (GF) post allogeneic stem cell transplant (allo-SCT) is potentially lethal. Salvage stem cells with or without additional conditioning regimen can be curative but concerns about toxicity and the need for adequate immunosuppression needs to be balanced in the therapeutic decisions. Due to the rarity of GF and paucity of data no consensus exists on the most preferred combinations to opt at the time of intervention. To address this unmet scenario we performed a large single institution retrospective study.
Methods- From January 1996- February 2016, 97 patients received treatment for GF following an allo-SCT. We excluded from the analysis patients (n-15) who received autologous cells as their sole rescue and those who developed GF after progression of the underlying malignancy. Both primary GF (48%) and secondary GF (52%) post 1st allo-SCT were included. Median time from 1st allo-SCT to GF rescue intervention was 56 (range 21-738) days. Conditioning regimen prior to allogeneic rescue cell infusions was categorized as : 1) no preparative regimen (21%) 2) single agent antithymocyte globulin (ATG) or Campath (6%) 3) Reduced intensity conditioning (RIC) chemotherapy or low dose total body irradiation (TBI) (200cGY) (28%) (4) Fludarabine (Flu) + ATG (41%) and 5) miscellaneous other combinations (4%). Engraftment (absolute neutrophil count ≥ 500 for 3 consecutive days) and overall survival (OS) from the time of intervention were the main outcomes of interest. The following factors were considered for their association with primary outcomes following GF rescue intervention: 1) donor/ patient demographics, 2) disease status, 3) graft- source (related, unrelated donors, peripheral blood, bone marrow and umbilical cord blood), cell dose, graft modification (t cell deplete vs replete), level of human leucocyte antigen (HLA)/ABO matching between donor and recipient and 4) treatment related metrics (conditioning regimens and graft versus host disease prophylaxis).
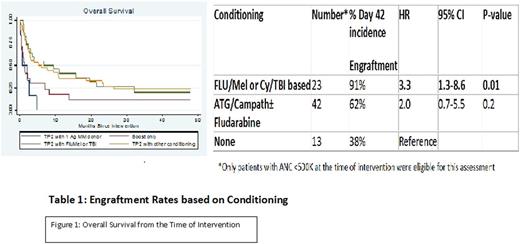
Results- Among patients (n=82) who received GF rescue intervention, 56 (68%) engrafted, 10 (12%) failed to engraft and 16 (20%) had early death (< 28 days). With a median follow up of 61 (range 11-242) months, 5-y OS was 18%. Only conditioning regimen correlated with engraftment with a significantly higher proportion of patients engrafting after Flu/Mel (92%) or TBI (91%) based preparative regimens (Table 1). In comparison, 38%, 40%, 67%, and 33% engrafted following no preparative regimen, and conditioning with ATG or Campath, Flu/ATG, and miscellaneous other group, respectively. Change of donor, graft source and graft modification were not significant predictors for engraftment. On multivariate Classification and Regression Tree (CART) analysis, use of 1 HLA antigen mismatched related or unrelated donor was associated with poor overall survival (HR 3.7, 95 % CI 1.5-8.9 P value 0.004). In the absence of 1 antigen related or unrelated donor the use of 2nd allo-SCT was associated with better survival compared with boost only (i.e. no preparative regimen prior to cell infusion) (HR- 0.5, 95 % CI 0.3-0.9, p value 0.03)(Figure-1). Graft rejection/failure (39.7%) and infections (23.5%) were the commonest primary causes of death.
Conclusions- GF post allo-SCT is a rare entity with sparse long term survivors despite interventions. For patients eligible to receive conditioning, use of RIC portends better engraftment and survival prior to cell rescue.
Oran: Celgene: Research Funding; AROG: Research Funding; Astex: Research Funding. Khouri: Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal